What
A set of tools for assessing the presence of coronary artery disease using non-invasive and automatic techniques for processing medical images.
Why
Myocardial ischemia, or coronary artery disease is the most common of the cardiovascular diseases and is one of the leading causes of death worldwide.
Up today, the standard diagnostic tools for myocardial ischemia are represented by invasive techniques, such as coronary catheterization, i.e. the insertion of a catheter in the coronary arteries. However, up to 40% of patients referred for coronary catheterization are found to have normal or near normal coronary arteries, and are thus subject to a costly and non-necessary invasive procedure.
Stress perfusion cardiac MR (SP-MRI) is a well-known non-invasive alternative to assess the myocardial perfusion, using a contrast agent to visualise myocardial blood flow. However, SP-MRI is still predominantly used only in experienced tertiary centres and research institutions, as the image analysis is observer-dependent, may involve complex acquisition protocols with double injections of the contrast agent, and frequently results in a significant underestimation of the extent of ischaemia.
Benefits
The proposed technology overcomes the afore-mentioned problems, by providing a set of tools that allow to fully automate the analysis of a patient heart, are completely operator-independent, objective and reproducible.
Moreover, the proposed technology allows a differential diagnosis of coronary heart disease and coronary microvascular disease (i.e. abnormal myocardial perfusion with angiographically normal large epicardial coronary arteries), which is an unsolved problem and leads to a high rate (up to 40%) of unnecessary invasive cardiac angiography.
Opportunity
The technology is protected by three patent families and is available for licensing. Suitable development partners are sought for commercialisation.
The Science
The proposed technology comprises
-
PDA: a method for the differentiation of coronary heart disease and coronary microvascular disease in SP-MRI, by detecting temporal and spatial inhomogeneities, also called “perfusion dyssynchrony”. Perfusion indexes are calculated from blood measurements taken on medical images along radial directions of the myocardium and/or on a plurality of layers in various regions of the heart; and
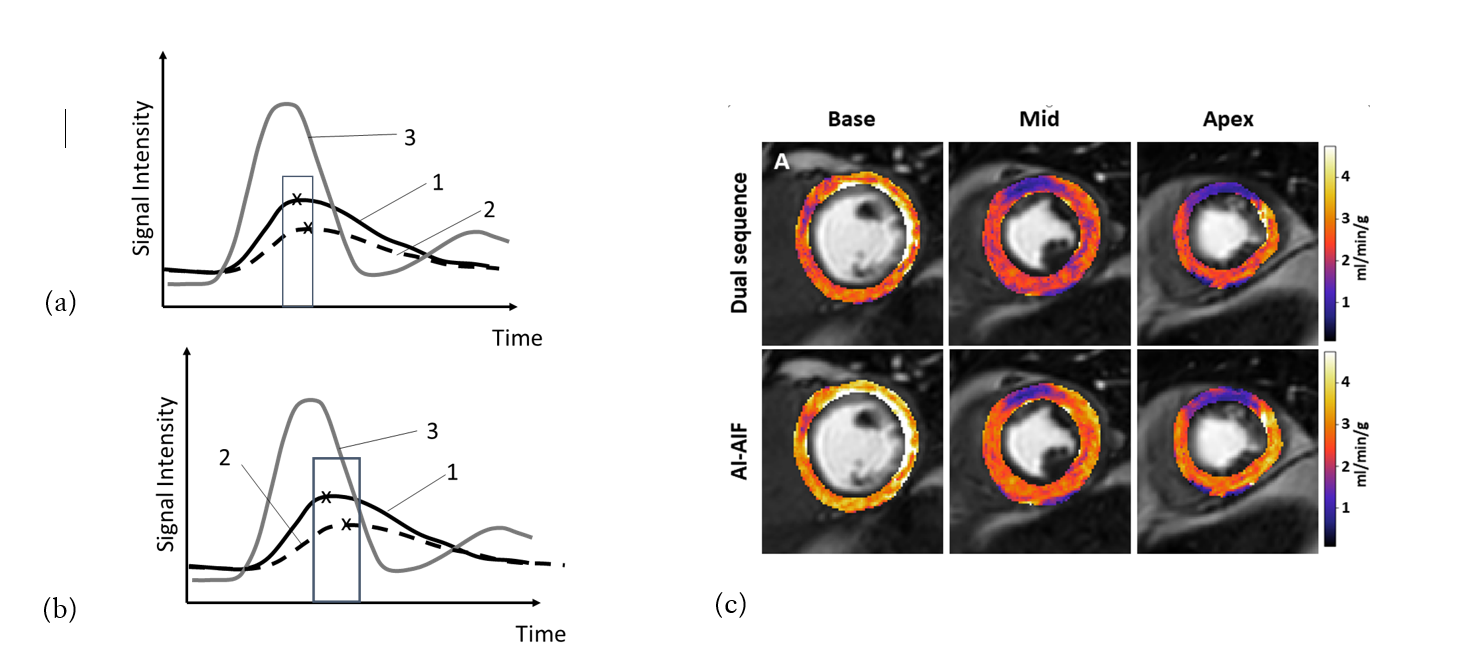
Figure:
Figs. (a) and (b) are examples of the PDA method output, as they show perfusion signal intensities over time measured respectively in a normal heart (Fig. (a)) and in an ischemic hearth (Fig. (b)). The light grey curve (3) represents the signal measured at a reference point in the left ventricle, the solid black curve (1) represents the signal measured in the epicardial layer and the dashed black line (2) represents the signal measured in the endocardial layer. The time to peak intensity (TTPI) is expected to be similar or vary over only a small range in a normal heart, as illustrated in Fig. (a). In case of ischemia, there will be an inhibition of the flow of blood through the myocardium, giving rise to a more significant difference or spread between the TTPIs between the various layers and the reference point, as illustrated in Fig. (b). The TTPI index in this case is positive, indicative of ischemia in a patient. A similar analysis can be carried out on radial segments.
Fig. (c) shows a comparison of quantitative myocardial blood flow maps obtained through SP-MRI with both a dual sequence acquisition protocol, wherein each image is obtained after a dual injection of contrast agent, and the AI-AIF model.
Patent Rights
PDA is protected by:
AI-AIF is protected by:
Further Information
Chiribiri, A. et al., (2016), "Perfusion dyssynchrony analysis", European Heart Journal - Cardiovascular Imaging: 17(12), pp. 1414–1423, doi:10.1093/ehjci/jev326.